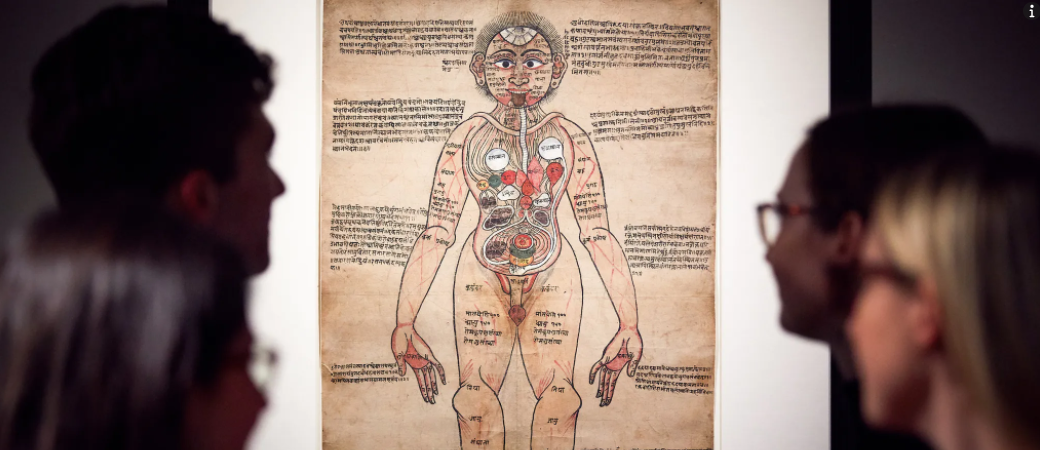
“A Pilot Study to Understand the Role of Medical Humanities in Medical Education”
September 26th, 2022
Clark Pitcher, Arya Prasad, Daniel Marchalik, Hunter Groninger, Lakshmi Krishnan and Michael Pottash study the perception of the students enrolled in the Georgetown University Medical Humanities Initiative of the benefits of a medical humanities curriculum.…